Converting accounts receivable into cash demands a well-organized, systematic and focused approach that is designed to facilitate problem resolution instead of just basic information gathering. Effective documentation facilitates vital reference material that can be very handy when analyzing and resolving problems that might emerge in the future.
Flatworld Solutions' Medical Claims Process
Identifying Benchmarks across Varied Payers
To understand the cash disbursement process followed by varied payers, it is vital to establish the benchmarks around their processing patterns. Information pertaining to this is typically gathered through historical data and other references, such as previously-issued Denial mails, EOBs (Explanation of Benefits) that were paid out, Manuals and Newsletters.
The benchmark information should clearly illustrate the following:
- Processing time for claims raised by the carrier.
- Data requirements such as tax ID number, provider number, pay-to address, etc.
- Checklists required from the carrier for all blocks in the HCFA-1500 claim form.
- Documentation requested-referrals, attachments and any other documents.
- Varied plans which the player has deployed, and card copies of each.
Note that processing and payment delays are not built into the benchmark, since these generally arise due to improper submission of claims documents.
We are committed to offer a well-planned system to deliver on the medical claims process, which includes the following steps:
Step 1 - Identifying Claims Outside the Benchmark
Further to the benchmarks being established, we identify the medical claims that are outliers to the benchmark. This process is done on a weekly basis to determine the total volume and value of such claims. This helps in defining a broad pattern on the key issues impacting most of the claims.
Step 2 - Prioritizing Medical Claims for Action
Upon identifying the medical claims that are outliers to the benchmark, we next identify the claims that can be processed forward. Reports are used to identify the payer type and filing limit.
Step 3 - Problem Identification
This forms a crucial step where problems and resolution approaches for the various cases are analyzed and documented. Since the medical insurance process is governed by complex regulations, insurance companies have devised complex rules for the claims payout process. Navigating through any errors-by way of erroneous data entry, incorrect claims information or external processing delay, will therefore need to be managed carefully. Each of the problems will need to be researched well and solutions will have to be identified, depending on the nature of error. The resolution approach is also applied to other pending claims of a specific carrier to ensure timely closure.
Step 4 - Drafting an Action Plan
Once the problem pertaining to a claim is identified, the case is assigned to our calling team to confirm the findings and establish understanding on the reasons for claim rejection. We then prepare an action plan to determine ways for faster claim payment. An action plan will establish the necessary steps to be initiated, such as change of address letters, dispatching physicians' enrolment forms, corrected claims and any additional documents.
Step 5 - Implement the Solution to all Outstanding Claims
Upon drafting the action plan to address specific problems, we create a solution approach that can be applied across all outstanding claims that fit within the specific problem category.
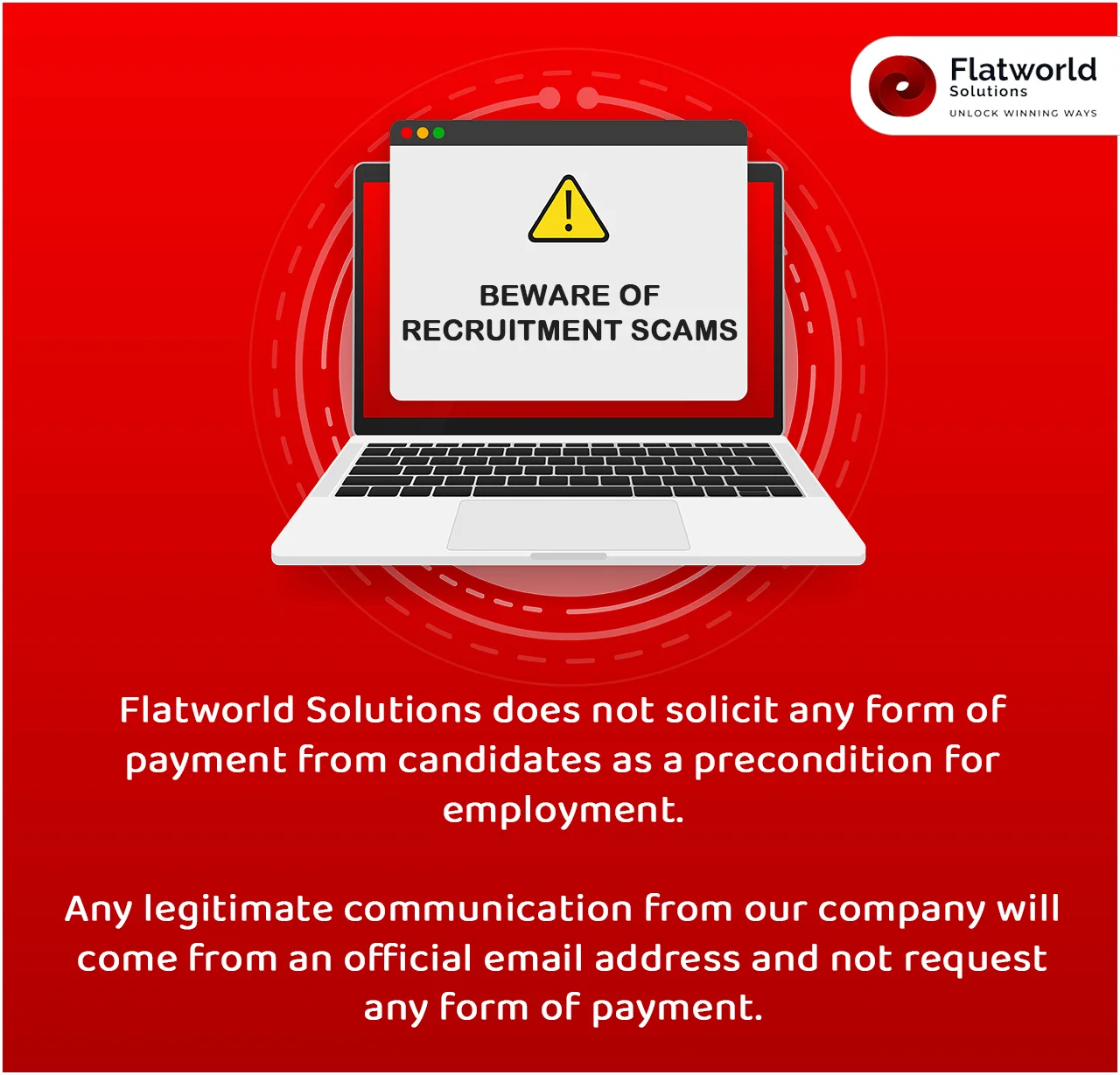
Outsource Medical Claims Processing Services to Flatworld Solutions
Are you looking for high quality and well-managed medical claims processing services? Try our world-class outsourcing services. Find out more about our key competencies, high quality infrastructure , competitive pricing and benefits.
To learn more about outsourcing your medical claims processing services to Flatword Solutions, please fill in the inquiry form , and our Client Engagement team will contact you within 24 hours.
Our Customers




Key Differentiators
AHIMA Healthcare Convention 2016
USA
Flatworld Solutions
116 Village Blvd, Suite 200, Princeton, NJ 08540
PHILIPPINES
Aeon Towers, J.P. Laurel Avenue, Bajada, Davao 8000
KSS Building, Buhangin Road Cor Olive Street, Davao City 8000
INDIA
Survey No.11, 3rd Floor, Indraprastha, Gubbi Cross, 81,
Hennur Bagalur Main Rd, Kuvempu Layout, Kothanur, Bengaluru, Karnataka 560077