According to the American Hospital Association, denial rates range from 10-15%. Hence, hospital denial management remains a significant challenge. This translates to billions of dollars in lost revenue annually. The Advisory Board's findings indicate that 90% of denied claims are preventable, yet hospitals only recover about 60% on average. These statistics underscore the pressing need for advanced denial management strategies to mitigate financial losses and improve operational efficiency.
The primary reasons for denials include complex payer regulations, documentation deficiencies, and coding inaccuracies. As healthcare reimbursement models evolve, these challenges become more pronounced. Administrative complexities alone account for 15% of all denials, as highlighted by Change Healthcare's 2023 study. Addressing these root causes requires a sophisticated approach that leverages advanced technologies and methodologies to streamline hospital denial management process and reduce errors.
Hospital Denials Management Best Practices
Effective denial management in healthcare has profound financial implications, potentially recovering up to 90% of initially denied claims. Advanced strategies transform hospital finances by enhancing revenue cycles and reducing administrative burdens. Operational efficiency is also improved through streamlined denial management workflows and reduced error rates, allowing healthcare providers to focus more on patient care and less on administrative tasks.
-
Harnessing Advanced Denial Analytics
Big data analytics can uncover hidden patterns in denial reasons by analyzing vast amounts of data from multiple sources. Advanced algorithms can identify correlations and trends that manual analysis might miss, providing insights into systemic issues and areas for improvement. Accurate categorization of denials is crucial for effective management.
Advanced categorization techniques use machine learning to continuously refine and improve the precision of denial categorization, ensuring that each denial is addressed appropriately and effectively. Using AI, one can predict potential denials while analyzing historical data and identifying risk factors. Similarly, ML models generate alerts for claims that are likely to be denied, allowing healthcare providers to proactively address issues before submission. Longitudinal data analysis provides insights into denial trends over time.
By understanding these trends, hospitals can implement strategic changes to policies and procedures, ultimately reducing the occurrence of denials and improving overall financial performance.
-
Revolutionizing Documentation and Coding Accuracy
AI-enhanced documentation tools can auto-populate clinical documentation, reducing the burden on healthcare providers and minimizing errors. These tools can verify the accuracy and completeness of documentation in real-time, ensuring compliance with payer requirements. Implementing real-time auditing systems allows for continuous monitoring and correction of documentation errors. These systems provide immediate feedback, enabling healthcare providers to address issues promptly and reduce the likelihood of denials.
Regular training and certification programs on advanced coding standards are essential for maintaining high accuracy rates. Peer reviews and coding audits help ensure that coding practices meet the latest industry standards and payer requirements. Automated coding solutions enhance efficiency by reducing manual effort and minimizing errors. Verification steps integrated into the automated process ensure that codes comply with payer requirements, further reducing the risk of denials.
-
Optimizing the Claims Submission Process
Optimizing the entire claims submission process involves mapping out each step, identifying bottlenecks, and implementing solutions to streamline workflows. This holistic approach ensures that claims are processed efficiently and accurately, reducing the likelihood of errors and denials. Robotic process automation (RPA) can handle repetitive tasks in the claims submission process, such as data entry and validation.
By automating these tasks, hospitals can improve efficiency, reduce human error, and allow staff to focus on more complex and value-added activities. Advanced pre-submission validation systems check claims for errors and compliance with payer requirements before submission. These systems use sophisticated algorithms to identify potential issues, allowing healthcare providers to correct them proactively.
Real-time feedback systems provide immediate alerts for any errors or discrepancies in claims. This proactive approach enables healthcare providers to address issues before submission, reducing denial rates and improving claim acceptance.
-
Innovative Denial Tracking and Reporting
Integrated denial management platforms provide a centralized system for tracking and managing denials. These platforms offer comprehensive visibility into denial patterns and trends, enabling healthcare providers to implement targeted interventions. Seamless integration with Electronic Health Records (EHR) ensures data consistency and accessibility. By leveraging EHR data, hospitals can enhance the accuracy of denial tracking and streamline the overall denial management process.
Cutting-edge dashboards offer real-time monitoring of key denial metrics. Customizable views allow different stakeholders to access the information most relevant to their roles, facilitating informed decision-making. In-depth analytical reports provide actionable insights for continuous improvement. These reports highlight trends, identify root causes, and suggest targeted interventions to reduce denial rates and improve financial performance.
-
Strategic Appeals Management
Automating the appeals process enhances efficiency and accuracy. Automated workflows streamline repetitive tasks, ensuring that appeals are processed promptly and correctly. Leveraging data to build strong, evidence-based appeal cases improves the likelihood of successful appeals. Analytical insights can support arguments and provide the necessary documentation to substantiate appeals.
-
Automated Follow-up Systems
Automated follow-up systems ensure prompt and consistent follow-up on appeals. These systems track the status of appeals and send reminders, reducing the risk of missed deadlines and lost appeals. Dedicated appeals teams focus solely on managing and resolving appeals. Specialized expertise improves appeal success rates and ensures that appeals are handled efficiently and effectively.
The Conclusion
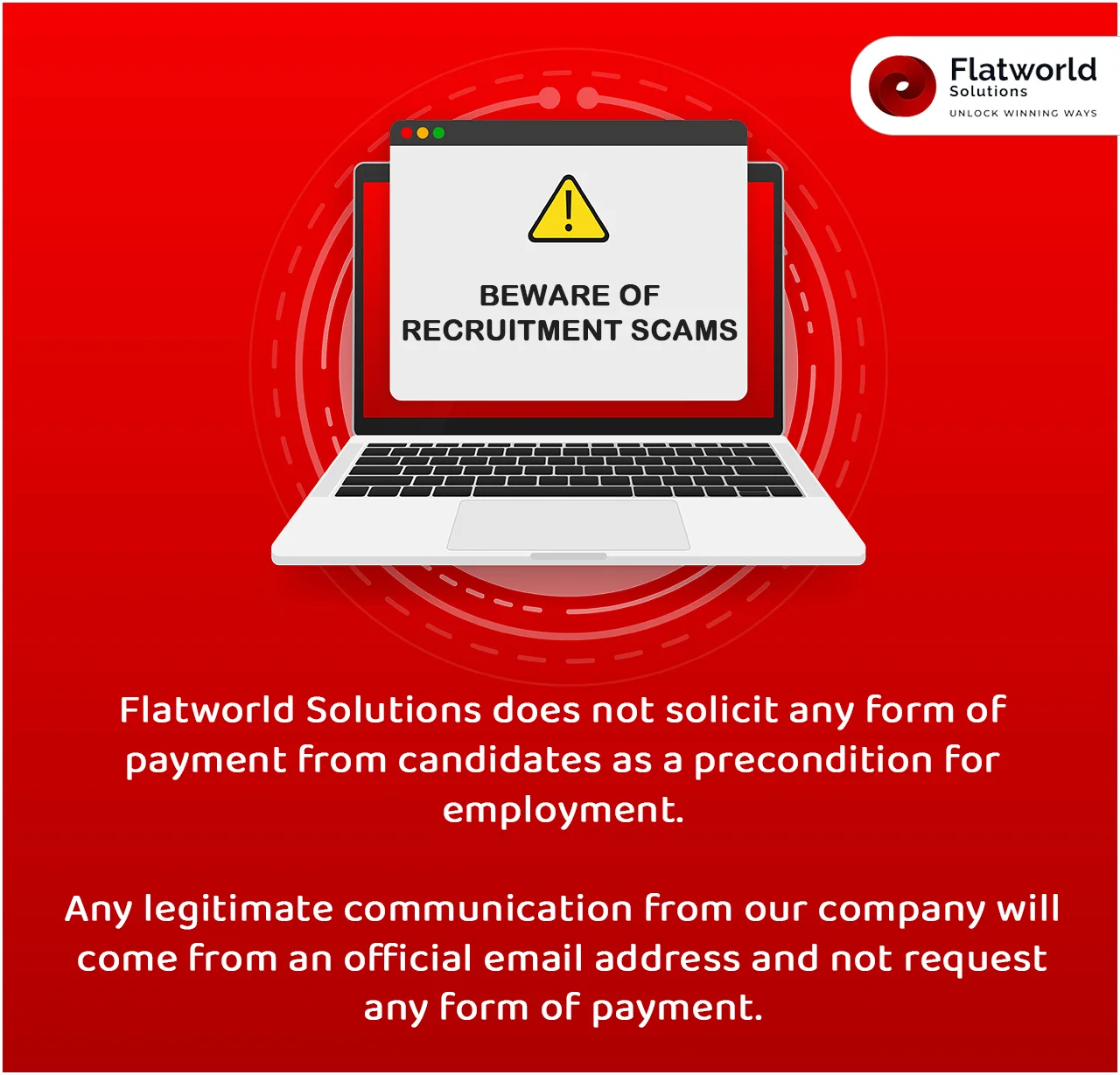
When selecting a medical claims denial management services company, evaluate their experience and success in the healthcare industry. Make sure they have a proven track record of reducing denial rates. Choose a partner offering tailored solutions, not generic approaches. Assess their technological capabilities, focusing on their use of AI, machine learning, and predictive analytics.
Ensure they provide continuous education and robust support for your staff, along with transparent, real-time reporting mechanisms. Additionally, prioritize their compliance with HIPAA and other data security standards to safeguard patient information. By considering these factors, you can select a company that meets your specific needs and supports your long-term financial and operational goals.
Contact UsOur Customers




Key Differentiators
AHIMA Healthcare Convention 2016
FAQs
USA
Flatworld Solutions
116 Village Blvd, Suite 200, Princeton, NJ 08540
PHILIPPINES
Aeon Towers, J.P. Laurel Avenue, Bajada, Davao 8000
KSS Building, Buhangin Road Cor Olive Street, Davao City 8000
INDIA
Survey No.11, 3rd Floor, Indraprastha, Gubbi Cross, 81,
Hennur Bagalur Main Rd, Kuvempu Layout, Kothanur, Bengaluru, Karnataka 560077